Rising cancer costs are driving health care budgets to unprecedented levels, but early detection can dramatically reduce both the human and financial costs of cancer. HAA's employer briefing on cancer prevention and screening revealed ways that employers can take action.
At the Health Action Alliance's Oct. 16, 2025, employer briefing on cancer prevention, business leaders and public health experts explored strategies to offset escalating treatment costs while protecting employee health. The conversation revealed how employers can leverage their position as trusted health authorities to encourage screening and preventive care, reducing excess health care spending and ultimately saving lives.
Read on for key insights and watch the full recording here.
Sarah Rauzin, Director and Lead of Research and Advisory at Meteorite and the Health Action Alliance, began the event with an overview of the current landscape of cancer in the U.S. today.
Cancer costs are spiraling across multiple dimensions. Cancer ranks as the number one driver of employer health care costs, with average treatment expenses reaching $10,000 per patient monthly and totaling an estimated $222 billion annually in the U.S. Beyond medical costs, 45% of cancer survivors report needing to miss or stop work due to physical symptoms, creating compounding productivity losses.
The pandemic created lasting disruptions in preventive care. COVID-19 caused routine screenings and early detection services to plummet, while rising misinformation and health care skepticism worsened the problem. A 2025 survey revealed just over half of eligible adults participated in routine cancer screening in the past year, a 10 percentage point drop from the year before. Among those patients who are behind on appointments, one in seven report feeling skeptical of the health care system, a 38% increase from 2024. One major insurance carrier found that over half of catastrophic claims exceeding $50,000 were from people who hadn't received a screening appointment in the past year.
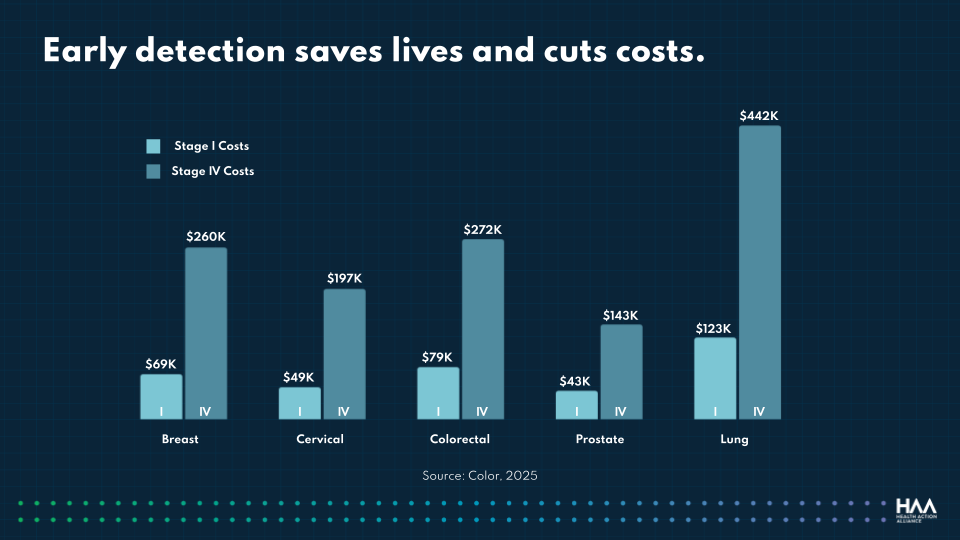
Early detection delivers dramatic cost savings. First-year treatment costs following diagnosis are significantly lower for stage 1 compared to stage 4 diagnoses, with cost savings ranging from $100,000 for prostate cancer to over $300,000 for lung cancer. These figures underscore early detection as both a moral and financial imperative.
Prevention goes beyond screening and eliminates risk factors. While early screening helps to catch cancer at a less developed stage, preventive interventions can eliminate the conditions that can increase someone’s risk for cancer, such as smoking or vaping, excessive drinking, worksite health hazards, and missed vaccines.
Lori Hoffman, Vice President of Product and Content Strategy at Meteorite and the Health Action Alliance, moderated a conversation with Millicent Gorham, CEO of the Alliance for Women's Health and Prevention, and Dr. Karen van Caulil, President and CEO of the Florida Alliance for Healthcare Value.
Multiple factors are driving the increase in cancer costs. Beyond later diagnoses due to fewer and later screenings, employers also face higher costs due to:
Rates are increasing fastest for women under 65. The World Health Organization predicts new cancer cases will increase by nearly 50% in North America by 2050, with rates climbing fastest for women under age 65. Additionally, shifting life patterns play a role — later age for first pregnancy and decreased breastfeeding show clear linkages to higher rates of breast cancer.
Women face unique barriers to preventive care. An Alliance for Women's Health and Prevention survey found that 42% of women are forgoing preventive health care screenings, annual checkups, tests, treatments, and vaccines, and having trouble getting appointments. Women cited inability to afford out-of-pocket costs, not feeling they needed care, and caregiving responsibilities for family members and children as major reasons for skipping screenings. Gorham emphasized, "Women are the chief medical officers of their families and their communities. And listen, if mama goes down, everybody goes down."
Obesity is a critical but often overlooked cancer risk factor. As obesity rates have increased for women, so have cancer cases. Obesity is a risk factor for numerous cancers, including breast, endometrial, ovarian, colorectal, esophageal, kidney, and pancreatic cancer. Van Caulil urged employers with active weight management strategies to "also think of it as a cancer strategy."
Insurance coverage gaps undermine screening participation. Beyond initial mammograms, secondary MRI or ultrasound screenings for conditions like dense breast tissue often aren't covered at zero cost, deterring women from pursuing follow-up care that could be lifesaving. Gorham stressed that comprehensive coverage "makes them feel valued as an employee and makes them want to be there as a productive employee."
Vaccine misinformation threatens cancer prevention progress. The spread of false information is leading to lower vaccine rates across the board and a resurgence in once-controlled diseases. Critically, misinformation about one vaccine type, like COVID vaccines, negatively impacts attitudes about others, including HPV and hepatitis B vaccines that prevent multiple cancers.

Supporting employers in taking immediate action on cancer prevention and screening:
Sign up for our newsletter to keep updated on HAA’s latest initiatives, insights and recommendations, and be first to receive new resources and event invitations.
Sign up